Researchers at the University of Ottawa Heart Institute (UOHI) have discovered gold nanoparticles and synthesized peptides restore function, contractility, and electrical conductivity to damaged heart tissue – a scientific feat which may one day be applied to save human lives.
The breakthrough research made the cover of the March issue of ACS Nano, a monthly, peer-reviewed, scientific journal of the American Chemical Society.
The heart attack vs. heart failure paradox
Dr. Marcelo Muñoz, a chemist in the Bio-Engineering and Therapeutic Solutions (BEaTS) Laboratory at the UOHI, and the primary author of the study along with fellow researcher, scientist and PhD candidate Cagla Eren Cimenci, said heart attack survivors are increasing thanks to leaps in scientific innovation, technology, and patient care. On the other hand, many heart attack survivors go on to develop an often-fatal condition called heart failure, which results from injuries sustained during the attack.

When a heart attack (myocardial infarction) occurs, one or more of the coronary arteries shut down, cutting off blood supply, nutrients, and oxygen to cells (cardiomyocytes) on the heart. Without rapid intervention, the affected tissue is lost and cannot be recovered. A scar forms on the heart and, over time, the muscle weakens, until ultimately, it fails. Patients with heart failure are no longer capable of pumping enough blood to meet their bodies’ demands.
Paradoxically, as deaths from heart attacks drop off, deaths from heart failure are on the rise. In Canada, as many as 750,000 people live with heart failure and 100,000 are diagnosed with the condition each year. Such staggering figures present scientists like Dr. Muñoz with important questions: Is a therapeutic solution capable of recovering damaged heart tissue even possible, and if so, can scientists use one to prevent a heart attack patient from becoming a patient with heart failure?
To date, no such therapy exists. However, early tests in mice are proving demonstratively positive.
Searching for a heart of gold
Gold nanoparticles – that is, tiny flecks of gold so small they are invisible to the naked eye – have been of keen interest to scientists for years. Their properties make them ideal for use in a variety of applications, including in electronics, nanotechnology and biomedicine.

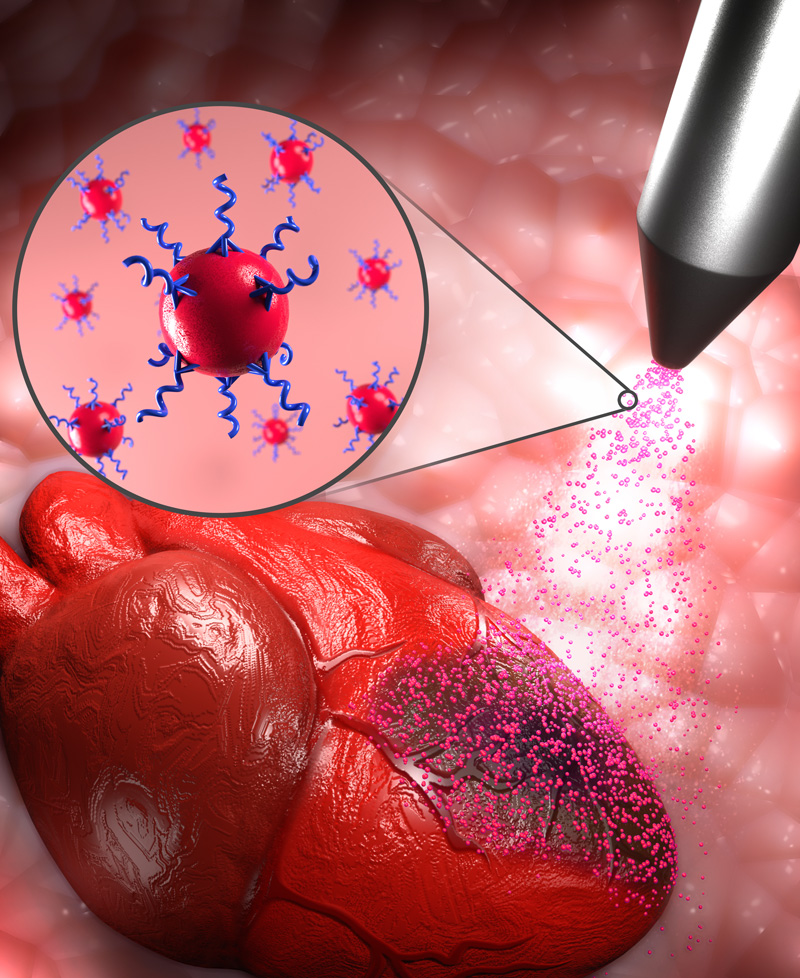
Muñoz and his colleagues encapsulated and stabilized these tiny golden nanoparticles with nanoengineered peptides (strings of amino acids). The peptides were fortified with spider-like branches that stem outward from their core. Then, by using a specially designed micro-nozzle (imagine a can of spray paint with a tip so fine it could deliver the application within micrometres), the nanoparticle and peptide solution was sprayed onto a localized area of the heart.
“When applied to mouse hearts, one week after infarction, the spray-on treatment resulted in an increase in cardiac function (2.4-fold), muscle contractility, and myocardial electrical conductivity,” writes Dr. Muñoz and his colleagues. “Our cumulative data suggest that the therapeutic action of our spray-on nanotherapeutic is highly effective, and in practice, its application is simpler than other regenerative approaches for treating an infarcted heart.”
Researchers have studied stem cell injections, cardiac patches, exosome delivery, and drugs, but these approaches to myocardial tissue regeneration have not yet translated into the clinic. Stem cell therapies offer great promise for new medical treatments; however, the process is costly and can take months. The gold nanotherapeutic system developed at the UOHI can be stored in the fridge, is ready to use when required, remains stable over time, and is a fraction of the cost.
It may be a long time before the science is ready for human trials, but Muñoz and his colleagues believe their discovery has groundbreaking potential.
“We may one day be able to stop the progression of heart failure in humans and return an affected human heart to its typical function after a heart attack,” said Muñoz. “Preventing a heart attack patient from becoming a heart failure patient is now not only a scientific possibility, but we may see it within our lifetime.”
Scientists in the BEaTS Laboratory at the UOHI, under the direction of Dr. Emilio Alarcon and Dr. Erik Suuronen, will next seek to reproduce and validate their result in further trials.

